Imagine a future where emergency responders carry life-saving blood in a backpack, available for immediate transfusions in both accident scenes and combat zones. Recent breakthroughs have paved the way for a freeze-dried, shelf-stable artificial blood substitute that can be rehydrated instantly. Such innovations not only mitigate the challenges associated with donor blood shortages but also provide a critical solution in time-sensitive emergencies.
Because this technology eliminates the need for refrigeration and cumbersome blood type matching, it represents a major leap forward in emergency medicine. Most importantly, it promises to transform trauma care, offering rapid, on-site treatment when seconds matter. This transformative research has captured global attention, as detailed in resources such as CBS News and WWNO.
Why Artificial Blood Matters
Natural blood supplies can be unpredictable and insufficient, particularly in regions with limited healthcare infrastructure. Because donor blood faces issues like perishability and strict temperature controls, emergencies often encounter delays that can prove fatal. In many scenarios, such as severe trauma from accidents or combat injuries, time is the enemy. Therefore, an immediately available alternative is essential to save lives.
Moreover, artificial blood addresses the chronic shortages that hospitals face regularly. Transitioning to this innovative substitute could alleviate the pressures on blood banks, ensuring that every emergency—whether in urban centers or remote locations—gets timely medical intervention. In addition, the technology is evolving quickly, as highlighted by reports in ASH Clinical News, promising a future where reliance on donor blood is greatly reduced.
How Artificial Blood Works: The Science Behind the Innovation
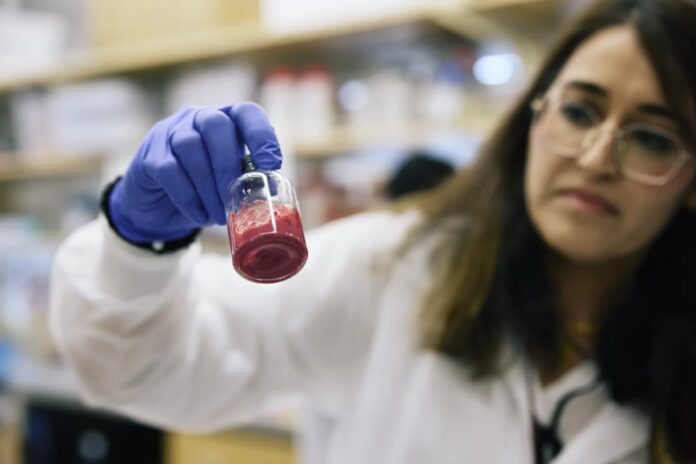
Scientific advancements have focused on creating substitutes that mimic natural blood functions, most importantly oxygen transport and circulation. Researchers have developed methods to extract hemoglobin from expired donor blood and encapsulate it in synthetic or fat-based nanoparticles. This innovation results in a stable, paprika-like powder that can be stored in sterile IV bags for extended periods. Whenever needed, medics simply add water to rehydrate the mixture into an injectable transfusion.
Because the rehydration process is both quick and efficient, the artificial blood is suitable for on-the-spot administration during emergencies. Furthermore, the technology is being refined continuously to improve its performance under various conditions. For more detailed insights on how these nanoparticles work, you can refer to the analysis provided in the University of Maryland’s breakthrough research video that demonstrates the rehydration and application process in a controlled setting.
On-the-Spot Usage: A Game-Changer for Emergencies
Utilizing artificial blood on the battlefield or at accident sites is a true game-changer. Because the product is shelf-stable at room temperature for years, medics can store a ready supply in ambulances, helicopters, or even in personal backpacks. This capability eliminates the delays associated with transporting refrigerated donor blood, thereby ensuring that trauma victims receive treatment without unnecessary wait times.
Besides that, the ability to administer blood directly at the injury site is poised to reduce mortality rates significantly. Each minute saved in emergency care can dramatically improve survival odds. As covered by The Week, deploying such innovative solutions in critical settings could revolutionize how we manage trauma and catastrophic injuries around the globe.
The Military’s Interest and Government Backing
The military has shown immense interest in this technology. Most importantly, the U.S. Department of Defense along with DARPA have invested heavily in accelerating the development and testing of artificial blood. Their objective is clear: to ensure that soldiers have immediate access to life-saving treatments on the battlefield, minimizing fatalities due to hemorrhagic shock.
Because rapid transfusion can mean the difference between life and death in combat scenarios, government backing has been instrumental in advancing this research. The robust funding and partnership with scientific institutions have created a conducive environment for innovation, as noted in the comprehensive reports by both ASH Clinical News and WWNO.
From Laboratory to Real-World Testing
Translating laboratory success into real-world application is a critical step for artificial blood. Initial animal studies have demonstrated that the rehydrated substitute successfully restores circulation and oxygen delivery comparable to natural blood. These encouraging results have paved the way for early human trials conducted in various countries, including Japan, where clinical tests are underway with universal artificial blood products suitable for any blood type.
Because these trials are meticulously designed, researchers can gauge both the efficacy and long-term safety of the new formulation. Moreover, the ongoing clinical evaluations are a testament to the scientific community’s commitment to addressing pressing healthcare needs. For those interested in following the progression of these studies, recent updates can be found in pieces such as CBS News, which outlines the evolving landscape of artificial blood research.
Challenges Ahead
Although the promise of artificial blood is immense, several challenges lie ahead. Because blood carries out a multitude of functions beyond oxygen transport, including immune responses and clotting, replicating these complex activities remains a significant scientific hurdle. Researchers must ensure that the substitute is not only effective in emergency situations but also safe for long-term use in diverse patient populations.
Therefore, rigorous regulatory reviews are essential to validate the product’s safety and functional equivalence to natural blood. Most importantly, extensive clinical trials must confirm that the benefits outweigh any potential risks. As emphasized in ongoing discussions within the biomedical community, overcoming these challenges will require comprehensive research and collaboration across multiple sectors.
Potential Impact: A Revolution in Global Health
The development of artificial blood could herald a revolution in global health. Because it promises to reduce deaths from traumatic injuries, especially in remote and under-resourced areas, its impact could be profound. Rapid transfusions could stabilize critical patients before they are transported to healthcare facilities, thereby saving lives that might otherwise be lost due to treatment delays.
Furthermore, this innovation could lessen the burden on blood banks and reduce the logistical challenges of traditional blood storage and transport. In regions prone to disasters or conflicts, having a reliable, on-demand blood substitute is invaluable. As outlined by several experts in The Week, these innovations may ultimately lead to a more resilient and adaptive global health infrastructure.
The Road Ahead
Ongoing innovation, brisk funding, and expanding clinical trials indicate that the dream of shelf-stable, on-demand artificial blood is nearer than ever. Because of the combined efforts of researchers, government agencies, and private investors, this technology is poised to change the landscape of emergency medicine permanently.
Most importantly, the progress being made today lays the groundwork for future breakthroughs in healthcare. With continuous improvement and diligent regulatory review, the gap between laboratory innovation and real-world application is closing swiftly. In the near future, both accident victims and combat casualties could benefit from this life-saving technology that offers a rapid, efficient, and universally applicable blood substitute.